Mini Review / Open Access
DOI: 10.31488/jjm.1000114
Meniscal allografttransplantation, still unaccepted treatment option in Japan? A review
Yuji Uchio*
Department of Orthopaedic Surgery, Shimane University, Japan
*Corresponding author:
Abstract
Once subtotal or total meniscectomy of the knee joint decreases tibiofemoral contact area leading to higher contact stresses, it deteriorates the cartilage resulting in faster progression of the osteoarthritis (OA). Because neither artificial implants nor autologous graftshave been established for the painful meniscus-deficient knees of young patients, meniscal allograft transplantation (MAT) has been thought to be a better alternative procedure to reduce higher stresses and prevent OA. In this paper, literatures concerning MAT are reviewed about the indications, contra-indications, meniscal allografts, complications, outcomes and rehabilitation. By presenting our experience, the medico-social problem of MAT in Japan is also discussed.
Keywords: meniscal allograft, transplantation, knee, Japan
Introduction
The menisci, a pair of wedged semilunar fibrocartilagesin the femorotibial joint of the knee are able to distribute loads and reduce the stresses, and play important roles of joint lubrication, proprioception, joint congruity, and knee stabilization[1].Total meniscectomy induces twice, or three times of the stresses, and even partial meniscectomy has a higher risk of cartilage injuries in young athletes[2,3]. Because the meniscusis a mostly avascularfibrocartilage tissue suggesting little capability of regeneration, preservation of the meniscusis regarded essentialfor cartilage protection and prevention of osteoarthritis (OA)[3].Kawata et al. identified 83,105 patientswho underwent meniscectomy and/or meniscal repair from a national database in Japan between 2007 and 2015: 69,310 underwent meniscectomy; 13,416 underwent meniscus repair and 379 underwent both in a single admission[4]. They found characteristic trends where the popularity of meniscus repair increased rapidly at the expense of meniscectomy in Japan, and the proportion of meniscus repair exceeded that of meniscectomy in those younger than 30 years in 2015[4]. However, subtotal or total meniscectomy is not avoided for the treatment of the complex tears of degenerateddiscoid menisci. Even partial meniscectomy decreased clinical outcome scores over time in patients treated arthroscopically for symptomatic discoidmeniscus[5]. Although artificial implants[6] or autologous grafts such as patellar tendons or quadriceps tendons had been applied to substitute the meniscus[7], no evidence has been reported that they could restore thenormal load distribution function as the native meniscusfor a longtimeand prevent the progression of OA. In 1989,Milachowski et al.first reported the experimental studies and clinical cases of the meniscal allograft transplantation (MAT)[8]. They also indicated that a systemic rejection phenomenon does not seem to occur by MAT, and the transplanted meniscus is capable of healing[8]. Since then, MAT has been thought to be a better alternative treatment option for the meniscectomized knee for young patients[9,10]. In this paper, literatures about MAT are reviewed about the indications and contra-indications, meniscal allografts, complications, outcomes and rehabilitation. By presenting our experience, the medico-social problem of MAT in Japan is also discussed.
Indications and Contra-Indications for MAT
Patients aged 50 years younger with a history of subtotal or total meniscectomy and pain and/or click at the meniscectomized compartment are candidates for MAT[11]. A normal axial alignment, a stable joint and intact cartilageshowed better results of MAT[12-14].By contrast, patients with obesity (BMI>35), and systemic diseases (e.g. infection, collagen diseases, synovial chondromatosis) are not recommended for MAT[7].Young patients with open physis should not be candidates of MAT which damages the epiphysial plate. General cartilage degeneration of the knee joint, axial mal-alignment of the lower extremity, and/or unstable kneesarerelatively contra-indications of MAT[7]. Autologous osteochondral transplantation should be combined with MATfor a focal cartilage defect with the meniscectomized knee joint [11]. Varus and valgus knee might be treated with a concomitant or previously performedhigh tibial or distal femoral osteotomy on MAT[11]. In case of past history of medial meniscectomy with concomitant deficient anterior cruciate ligaments (ACL), ACL reconstruction should be recommended witha concomitant MAT to improve the results[13]. Prophylactic MAT for the meniscectomized knee joint does not guarantee the successto prevent the progression of OA and is not routinely recommended yet[15].
Meniscal Allograft
Meniscal allografts are preserved by four proceduresincluding cryopreservation, deepfrozen, fresh, and freeze-dried[9,15]. Freeze-dried meniscal allografts cannot warrant the restoration of the normal load distribution function as the native meniscus. To avoid the danger of transmission of infectious diseases and the impossibility to match the meniscal size, most meniscal allografts are deepfrozen or cryopreserved. An expensive cryopreservation techniquehas a risk of transmission of infectious diseasesdespite the complex process[15]. Because the viability of the graft cannot be confirmed to improve the morphological and biochemical characteristics of them, inexpensive deepfrozen meniscal allografts have advantages of little risk of disease transmission and the storage of the variable sizes[9,15].Although cryopreserved menisci had a higher elastic modulus and point of rupture compared to fresh frozen menisci [16], clinical results of MAT showed no significance between deepfrozen and cryopreserved meniscal allografts[13, 15].
Complications of Meniscal Transplantation
Arthrofibrosis, loosening of the bone plug of the meniscus, meniscal allograft tear or failure of the healing to the periphery after MAT were described in the literature[9, 11]. The general potential complications regardingsurgery and anesthesia, such as surgical site infection, deep venous thrombosis, and neurovascular injuries are similar in MAT as otherknee surgeries. Immune response might be caused at the allogenic bone attached with meniscus. Concerns regarding disease transmission, primarily of Hepatitis C, HIV, and prionn diseases can occur even when appropriate sterilization procedures have been performed for cryopreserved and deepfrozen meniscal allografts[7,15]. These risks are consideredsmall but must be discussed with the patient priorto intervention and informed consent should be given.Patients selection, deliberate planning, and careful rehabilitation are important to avoid complications and poor outcome after a meniscal transplantation.
Outcome
The allogenicmeniscus can be implanted by means of an open or an arthroscopically assisted technique. An open technique has advantages of good overview of the compartment and application of combined surgery such as osteotomies around the knee joint. By contrast,arthroscopically assisted techniques have minimum invasion, no disruption of the collateral ligament, and faster revalidation. In the literature, it remainsuncertain which has superiority regarding the outcomes, complications and chondroprotective effects between the open and the arthroscopic approach and the different fixation techniques[7,9,10].
Hergan et al. reviewed 14 studies with at least 2 years’ follow-up, validated outcome measures, and in which the allograft meniscal horns were secured with bony fixation[17]. According theirsystematic review, percent satisfaction rangedfrom 62.5% to 100% and the rates of radiographic narrowing of joint space of the transplanted compartment of the knee varied from 7.5% to 75%.Results of a second-look arthroscopy procedurewere described in 6 of the 14 articles,however, the studies contained onlya subset of the patient population. Failures of the meniscal allograft occurred at 2 years earlier, 2 years, and 2 years over ranged from7 to 11%, 12 to 35%, and 25 to 50%, respectively. The study by Wirth al. ofsix cases used deepfrozen meniscal allografts with a follow-up of 14 years, showed the Lysholm score was 84 +/- 12 points at 3 years postoperatively and 75 +/- 23 points at 14 years, although all allograft and articular cartilage underwent degenerative changes[18]. By contrast, Verdonk et al. reported a long follow up study of 42 meniscus allograft transplantations in 41 patients with a minimum follow-up of 10 years (minimum 10 years, mean 12.1 years), demonstrating that radiographical analysis revealed no further joint space narrowing in 13/32 knees (41%). Fairbank changes remained stable in 9/32 knees (28%)[19]. MRI analysis showed no progression of cartilage degeneration in 6/17 knees (35%). An increased signal intensity of the allograft was present, as was partial graft extrusion in the majority of patients at the final follow-up[19]. In their conclusion, progression of further cartilage degeneration or joint space narrowing was absent in a considerable number of cases, indicating a potential chondroprotective effect[19].Smith et al. reviewed thirty-eight studies with 1056 allografts and demonstrated that the weighted mean joint space loss was 0.032 mm at 4.5 years across 11 studies[20]. Meniscal extrusion was present in nearly all cases but was not associated with clinical or other radiological outcomes. Meniscal healing rates were high, although the size, shape and signal intensity were commonly altered from that of the native meniscus. They concluded that there is some evidence to support the hypothesis that MAT reduces the progression of osteoarthritis, although it is unlikely to be as effective as the native meniscus[20].
Contrarily, Van Der Straeten et al. studied 329 MATs in 313 patients, suggesting that MAT did not delay or prevent tibiofemoralOA progression [21]; 19.2% were converted to a knee prosthesis at a mean of 10.3 years. Patients younger than 35 with no-to-mild cartilage damage may benefit from MAT for relief of symptoms (survivorship 51.9% at 20.2 years), but patients and healthcare payers and providers should be aware of the high number of surgical re-interventions [21].
Rehabilitation
Rehabilitation is an important component to get success after MAT, however the protocol and program of rehabilitation after MAT have not been established[12]. It is still controversial on the timing with regards to tissue loading and returning to normal daily living or sports activities[10]. Lee et al. recommended early joint exercises and progressive weight bearing to achieve full range of motion (ROM) within 2 months and return to sports activities in 6-9 months[22]. The ROM exercises are administered according to the stage of rehabilitation. Closed kinetic chain exercises and patellar mobilization are encouraged. Open kinetic leg curl exercise that creates a suction cup effect is not allowed in the early rehabilitation stage[22,23]. Proprioception and neuromuscular control exercises are allowed immediately after surgery with a goal of performing light jogging by 4-6 months postoperatively and sports activities by 6-9 months postoperatively[22,23]. In the case of MAT with concomitant ACL reconstruction, rehabilitation protocol should be modified according to the protocol of ACL rehabilitation. ACL using hamstring tendons should not be encouraged to full extension immediately after surgery to avoid the stretch out of the ACL grafts. There is a dilemma between early active motion of knee joint preventing arthrofibrosisand knee immobilization for maturation of the transplanted grafts.
Case
A 42-year-old male who has a history of total meniscectomy 25 years ago after knee twist injury in the valley ball game, came to our clinic and complained severe left knee pain, click and giving way. Orthopedic examination revealed swelling and ballottement of the left knee joint, and meniscus sign at the lateral compartment. His preoperative ROM was 0° of extension and 140° of flexion. The anterior drawer sign (1+), Lachman test (1+), and pivot shift test (glide) were all positive according to the International Knee Documentation Committee form. The radiographic Kellgren–Lawrence classification was Grade 2 and the standing femorotibial angle (FTA) was 175° (Figure 1), and the Rosenberg’s view showed the diminished joint space of the lateral compartment.

Figure 1.Preoperative radiographs: (A) weight-bearing anteroposterior view, and (B) lateral view.
Preoperative proton density magnetic resonance imaging (MRI) showed a bucket-handle tear of the medial meniscus with absence of the ACL, the lateral meniscus diminished by total meniscectomy and a focal cartilage defect in the lateral femoral condyle (Figure 2).

Figure 2.Preoperative proton density MRI: (A) a bucket-handle tear of the medial meniscus (arrow) and the lateral meniscus diminished by total meniscectomy and a focal cartilage defect (*) of the lateral femoral condyle in the coronal view, and (B) in the sagittal view.

Figure 2(c).absence of the anterior cruciate ligament and a bucket-handle tear of medial meniscus (double PCL sign: arrow) in the sagittal view.
The Japanese Orthopaedic Association (JOA) and Lysholm scores were 50 and 15 points, respectively. Upon diagnosis of a painful totally-meniscectomized knee with a concomitant torn ACL and a focal cartilage defect of the lateral condyle, we had minutely planned MAT combined with ACL reconstruction and the osteochondral transplantation. Then wenegotiated perseveringly about this MAT plan with the Tokai Reginal Tissue Bank (Nagoya, Japan), that has supplied allografts such as bone-patellar tendons for allogenic ACL reconstruction and bone allografts for revision arthroplasties in more than 10,000 cases for over 10 years. The protocol of MAT was approved of the Ethical Committee of Shimane University School of Medicine and the operation was permitted by the Chugoku Regional Bureau of Health and Welfare in Japan.
Under general anesthesia, arthroscopy revealed that both the ACL and the lateral meniscus were absent, and bucket-handle tear of the medial meniscus and a focal cartilage defect (10x12mm) of the lateral femoral were noted (Figure 3).
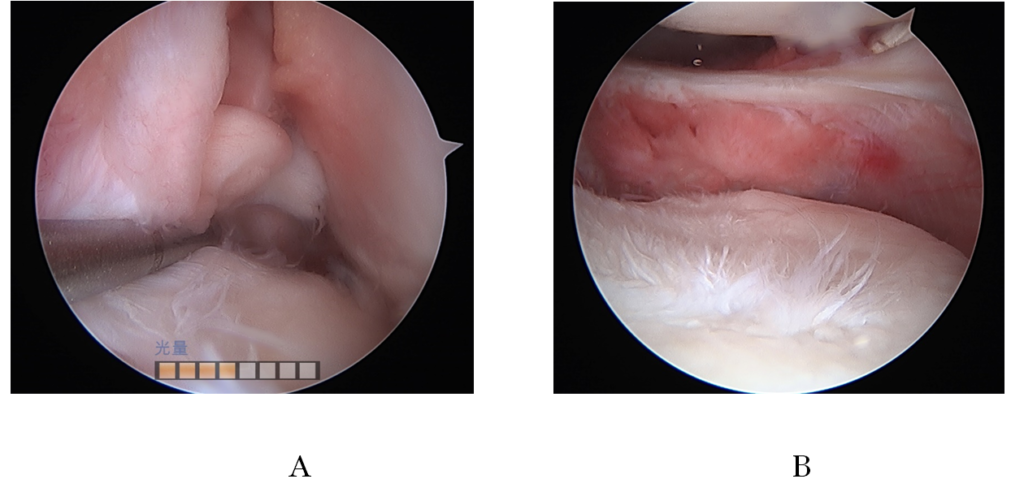
Figure 3.Arthroscopic findings: (A) absence of the ACL in the intercondylar space, (B) the lateral meniscus diminished by total meniscectomy in the lateral compartment. ACL: anterior cruciate ligament.
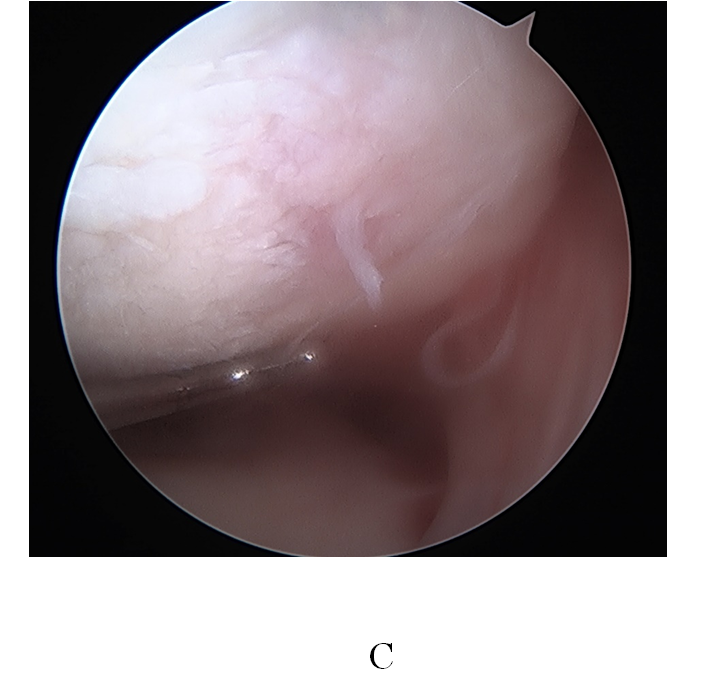
Figure 3(c). a focal defect of the cartilage of the lateral femoral condyle
First, medial meniscal suture was performed by an all-inside technique using three sutures of FastFix meniscal repair system (Smith & Nephew, Tokyo, Japan) under arthroscopy. Second, an ACL double-bundles reconstruction was performed by means of a transtibial technique using the two-strand semitendinosus tendons combined with the Leeds–Keio ligament and TightRope RT (Arthrex Inc., München, Germany; Figure 3). Bone tunnels were made in the femur [6 mm in diameter for anteromedial bundle (AMB), 5 mm for posterolateral bundle (PLB)] and in the tibia (7 mm in diameter for AMB, 6 mm for PLB). The graft length pattern was 2 mm over the top pattern. Third, an osteochondral graft was performed at the lateral femoral condyle using an osteochondral autologous transfer system (Acufex, Smith & Nephew, Andover, MA, USA). One 8.5 mm osteochondral graft was harvested from the non-weight-bearing area of the lateral femoral condyle (Figure 4A). In addition to the osteochondral transplantation, a microfracture was created around the osteochondral graft area of the lateral femoral condyle. Fourth, a deepfrozen meniscal allograft with bone supplied by the Tokai Reginal Tissue Bank (Nagoya, Japan) was applied to the lateral compartment and sutured to the peripheral capsule by three sutures of FastFix meniscal repair system (Smith & Nephew, Tokyo, Japan) and three sutures by all-inside technique using the Knee ScorpionTM suture passer (Arthrex Inc., München, Germany; Figure 4B,C,D, Figure 5B).
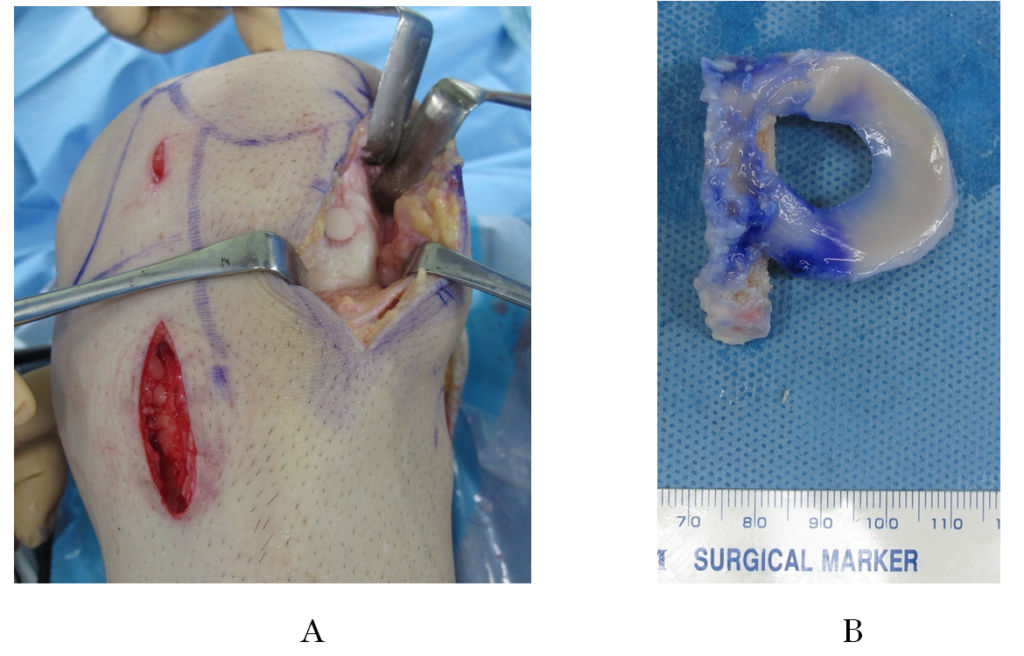
Figure 4.Surgical procedure: (C) insertion of the meniscal allograft and (D) fixation of the meniscal allograft combined with an osteochondral transplantation
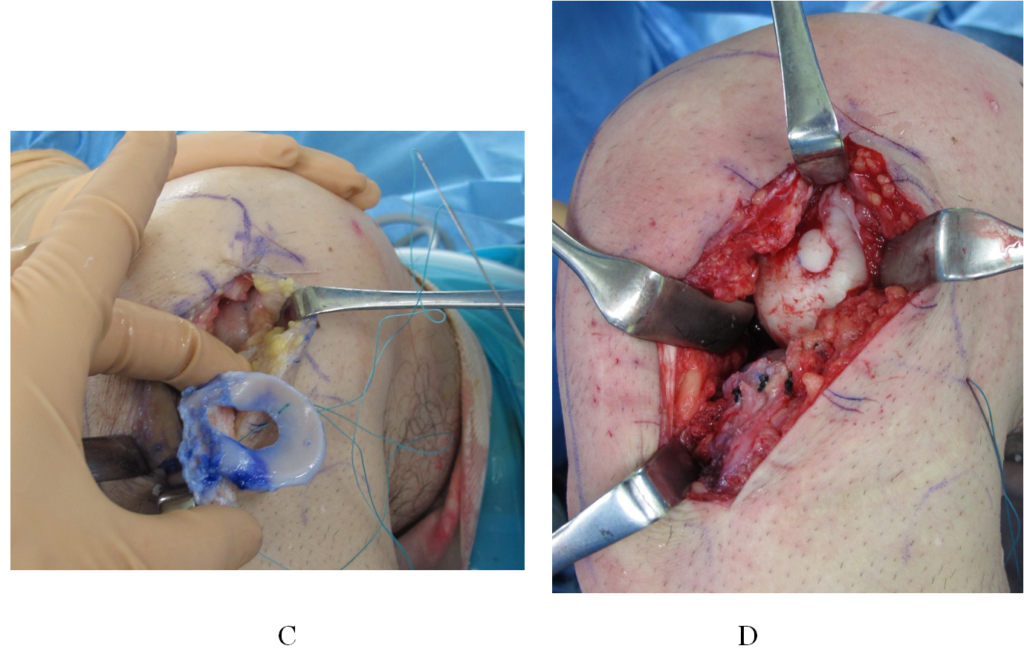
Figure 4(C,D).Surgical procedure: (C) insertion of the meniscal allograft and (D) fixation of the meniscal allograft combined with an osteochondral transplantation
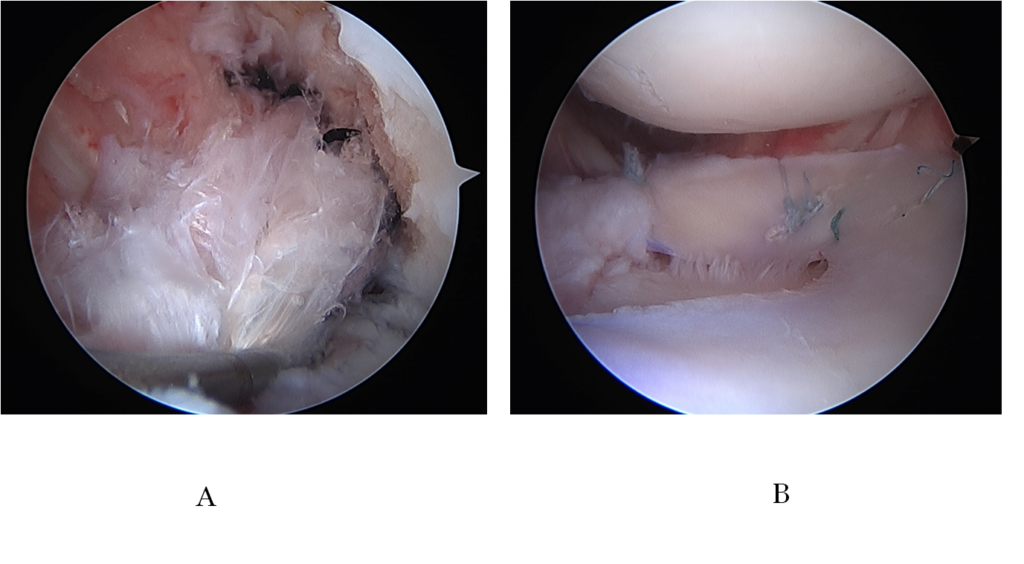
Figure 5.Arthroscopic findings: (A) double bundles ACL reconstruction in the intercondylar space, (B) the meniscal allograft transplantation in the lateral compartment. ACL: anterior cruciate ligament.

Figure 6.Postoperative radiographs at 1 year after surgery: (A) weight-bearing anteroposterior view, and (B) lateral view.
Finally, the tendons were fixed using double spiked staples (Meira, Gifu, Japan) at the anteromedial aspect of the tibia under 30 N load for the AMB and 10N load for the PMB at 10° of knee flexion.
ROM exercise started immediately at the next postoperative day, partial and full weight bearing walking started at 2weeks, and 4 weeks after surgery, respectively.At one year later, he complained neither pain nor click and could walk without giving way. Physical examination demonstrated neither swelling nor ballottement of the left knee joint despite a little limitation of the ROM(-10 to 135°)without any meniscus sign and anterior instability. He had no allergic symptoms and his blood-chemical test showed normal. The JOA and Lysholm scores at 1 year after operation were 93 and 99, respectively. Radiographs and MRI showed that lateral joint space was maintained, the reconstructed ACL was maturated, and the meniscal allograft and the osteochondral graft were fixed good in the lateral compartment (Figure 6 and 7). The patientwas able to return to occupation as a cook.
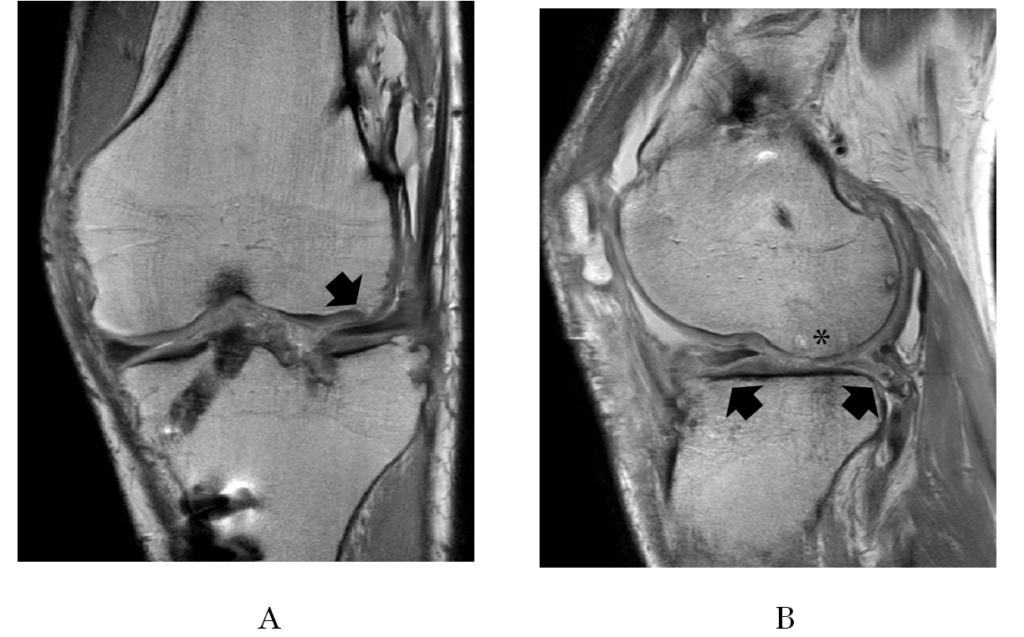
Figure 7.Postoperative proton density MRI at 1 year after surgery: (A) the fixed medial meniscus and the meniscal allograft in the lateral compartment (arrow) in the coronal view, and (B) the meniscal allograft in the lateral compartment (arrows) and an osteochondral transplantation (*) of the lateral femoral condyle in the sagittal view.

Figure 7(c).Postoperative proton density MRI at 1 year after surgery: (C) double bundles ACL reconstruction in the sagittal view.
Discussion
In Japan, this is the first report of MAT for the treatment of the knee after total meniscectomy. And it is also the first one of MAT combined with ACL reconstruction and osteochondral transplantation. In 1989, Milachowski et al. reported experimental and short-term results of the MAT technique as a potential treatment option in a painful meniscectomized knee[8]. Since then, many clinical, radiographical and MRI studies were published in the world concerning indications and contra-indications, graft type, preservation methods, complications, and combined surgeries[9,10,15, 17,18,20]. Contrarily,because of the failure of the first heart transplantation in 1968, no allograft had been clinically used in Japan for the medical treatment untilthe Organ Transplant Law went into effect in 1997. Between 1999 and 2016, organs from 530 brain-dead people were used for 2287 transplants, which involved hearts, lungs, livers, pancreases, kidneys and small intestines[24]. However, no meniscal allograftssupplied even from heart-dead people have been applied in general despite the huge number of meniscectomies in Japan[4]. Since 2016 All National Insurance has covered the cost of the meniscal allograft with bone from the tissue banksallowed by the Japanese Society of Tissue Transplantation.The Regional Bureau of Health and Welfare in Japan has permitted the medical institute doing MAT.However, the MAT is still a limited, nonstandard and complicated medico-social procedure in Japan.
Once the meniscus is completely lost, it is a consensus that the progression of OA is not avoided and causes pain reducing the physical and social function.Despite the good results of MAT in the short-term, no case of the treatment has been reported in Japan. For patients aged 60 years over, arthroplasty using artificial implants might be indicated. Indeed, for the relative younger patients the distal femoral varus osteotomy might be indicated for the lateral compartment with narrowing the joint space after subtotal or total meniscectomy[25]. However, varus femoral osteotomy might theoretically reduce the load of the lateral compartment of the knee joint, and it might cause overstress to the medial compartment resulting in the medial type of OA. Although osteochondral transplantation could reduce temporaly the load of the meniscectomized compartment, no substitute as the meniscus might cause unstable kinematics of the joint and deteriorate the cartilage again for a long time.Neither artificial implants nor autologous grafts have been reported to restore the normal load distribution function as the native meniscus for a long time and prevent the progression of OA. At present, MAT is certainly regarded as a better alternative treatment option for the painful meniscus-deficient knees of young patients. I believe that it is right now to start the MAT and accumulate data and build evidence in Japan.
Acknowledgement
The author deeply thanks patient who had the first MAT in Japan.The author also thanks Dr. Nobuyuki Kumahashi, Dr. Suguru Kuwata, and Dr. Hiroshi Takuwa for clinical assistanceof the surgery and patient’s care.
References
Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193 (Pt 2):161-78.
Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint:physical behavior of the knee joint with or without menisci. ClinOrthopRelat Res. 1980;(149):283-90.
Chahla J, Cinque ME, Godin JA, et al. Meniscectomy and resultant articular cartilage lesions of the knee among prospective National Football League players: An imaging and performance analysis. Am J Sports Med. 2018;46(1):200-207.
Kawata M, Sasabuchi Y, Taketomi S, et al. Annual trends in arthroscopic meniscus surgery: Analysis ofa national database in Japan. PLoS One. 2018;13(4):e0194854.
Haskel JD, Uppstrom TJ, Dare DM, et al. Decline in clinical scores at long-term follow-up of arthroscopically treated discoid lateral meniscus in children. Knee SurgSports TraumatolArthrosc. 2018.[Epub ahead of print].
de Groot JH. Polyurethane scaffolds for meniscal tissue regeneration. Med Device Technol. 2005 Sep;16(7):18-20.
Peters G, Wirth CJ. The current state of meniscal allograft transplantation and replacement. Knee. 2003;10(1):19-31.
Milachowski KA, Weismeier K, Wirth CJ. Homologous meniscus transplantation. Experimental and clinical results. IntOrthop. 1989;13(1):1-11.
Samitier G, Alentorn-Geli E, Taylor DC, et al. Meniscal allograft transplantation. Part 1: systematic review of graft biology, graft shrinkage, graft extrusion, graft sizing, and graft fixation. Knee Surg Sports TraumatolArthrosc. 2015;23(1):310-22.
Samitier G, Alentorn-Geli E, Taylor DC, et al. Meniscal allograft transplantation. Part 2: systematic review of transplant timing, outcomes, return to competition, associated procedures, and prevention of osteoarthritis. Knee Surg Sports TraumatolArthrosc. 2015;23(1):323-33.
Verdonk R, Almqvist KF, Huysse W, et al. Meniscal allografts: indications and outcomes. Sports MedArthrosc.2007;15:121-125.
Heckmann TP, Barber-Westin SD, Noyes FR. Meniscal repair and transplantation: indications, techniques, rehabilitation, and clinical outcome. J Orthop Sports PhysTher.2006; 36:795-814.
Lubowitz JH, Verdonk PC, Reid JB, et al. Meniscus allograft transplantation: a current concepts review. Knee Surg Sports TraumatolArthrosc. 2007; 15:476-492.
Getgood A, Robertson A. Meniscal tears, repairs and replacement – a current concept review. Orthop Trauma. 2010;24(2):121-128.
Moens K, Dhollander A, Moens P, et al. Meniscal transplantation: still experimental surgery? A review. ActaOrthop Belg.2014;80(3):403-13.
Ahmad S, Singh VA, Hussein SI. Cryopreservation versus fresh frozen meniscal allograft: A biomechanical comparative analysis. J OrthopSurg (Hong Kong). 2017;25(3).
Hergan D, Thut D, Sherman O, et al. Meniscal allograft transplantation. Arthroscopy. 2011;27(1):101-12.
Wirth CJ, Peters G, Milachowski KA, et al. Long-term results of meniscal allograft transplantation. Am J Sports Med. 2002;30(2):174-81.
Verdonk PC, Verstraete KL, Almqvist KF, et al. Verdonk R. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg SportsTraumatolArthrosc. 2006;14(8):694-706.
Smith NA, Parkinson B, Hutchinson CE, et al. Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports TraumatolArthrosc. 2016;24(9):2923-35.
Van Der Straeten C, Byttebier P, Eeckhoudt A, et al. Meniscal Allograft Transplantation Does Not Prevent or Delay Progression of Knee Osteoarthritis. PLoS One. 2016;11(5):e0156183.
Lee SR, Kim JG, Nam SW. The tips and pitfalls of meniscus allograft transplantation. Knee SurgRelat Res.2012;24(3): 137-145.
Rodeo SA. Meniscal allografts – where do we stand?AJSM. 2001;29(2): 246-261
Japan Organ Transplantation Network.
Sherman SL, Thompson SF, Clohisy JCF. Distal femoral varus osteotomy for the management of valgus deformity of the knee. J Am AcadOrthop Surg. 2018;26(9):313-324.
Received: May 10, 2018;
Accepted: May 29, 2018;
Published: May 31, 2018
To cite this article : Uchio Y. Meniscal allograft transplantation, still unaccepted treatment option in Japan? A review. Japan Journal of Medicine. 2018: 1:3.
© Uchio Y, et al. 2018.
