Review / Open Access
DOI: 10.31488/jjm.1000128
State of Art of Oral Vitamin B12 (Cobalamin) in Biermer’s Disease (Pernicious Anemia)
Emmanuel Andrès*1, Zulfiqar Abrar-Ahmad2, Thomas Vogel3, Georges Kaltenbach3
Department of Internal Medicine, Diabetes and Metabolic Diseases,Hôpitaux Universitaires de Strasbourg, Strasbourg,France.
Department of Geriatrics, CHRU de Rouen, Rouen, France.
Department of Geriatrics andInternalMedicine Universitaires de Strasbourg, Strasbourg, France.
*Corresponding author:Prof. E. Andrès, Service de MédecineInterne, Diabète et Maladies Métaboliques,Clinique Médicale B, Hôpital Civil – Hôpitaux Universitaires de Strasbourg,1 porte de l’Hôpital, 67091 Strasbourg Cedex, France, Tel: 3-33-88-11-50-66 ; Fax: 3-33-88-11-62-62 ;
Abstract
Management of cobalamin deficiency with vitamin B12 injections is currently well codified, but new routes of vitamin B12 administration (oral and nasal) are being studied. In the setting of Biermer’s disease, two prospective controlled randomized studies, a recent systematic review by the Cochrane group and fourprospective studies were found and provide evidence that oral vitamin B12 treatment may adequately treat cobalamin deficiency. The efficacy was particularly highlighted when looking at the marked improvement in serum vitamin B12 levels and hematological parameters, for example hemoglobin level, mean erythrocyte cell volume, reticulocyte count. The effect of oral cobalamin treatment in patients presenting with severe neurological manifestations has not yet been adequately documented. Oral cobalamin treatment avoids the discomfort, inconvenience and cost of monthly injections.
Keywords: Vitamin B12,cobalamin, oral vitamin B12,oral cobalamin,cobalamin deficiency,biermer’s disease, pernicious anemia, treatment, therapy
Introduction
Vitamin B12 (cobalamin) is the largest and most complex of all the vitamins [1]. Their molecular structure is C63H88CoN14O14P or C62H88CoN13O14P and their molecular weight is 1329.37 g/mol (Figure 1). The name vitamin B12 is generic for a specific group of cobalt-containing corrinoids with several essential biological activities in humans. Interestingly it is the only known metabolite to contain cobalt, which gives this water-soluble vitamin its red color. This group of corrinoidsis also known as cobalamins.
The main cobalaminsin humans and animals are hydroxo-, adenosyl- and methyl- cobalamin, the last two being the active coenzyme forms [2]. In fact, these compounds are necessary for hematopoiesis, neural metabolism, DNA and RNA production, and carbohydrate, fat, and protein metabolism.
To date, management of vitamin B12 deficiency with vitamin B12 injections is currently well established, but new routes of vitamin B12 administration, particularly oral and nasal, are being studied [3,4]. The treatment is based on cyano- and hydroxo-cobalamin in the form of tablets, injectable or oral solutions.
This narrative review summarizes the current knowledge on the efficacy and safety of oral vitamin B12 (cobalamin) therapy in Biermer’s disease (pernicious anemia).
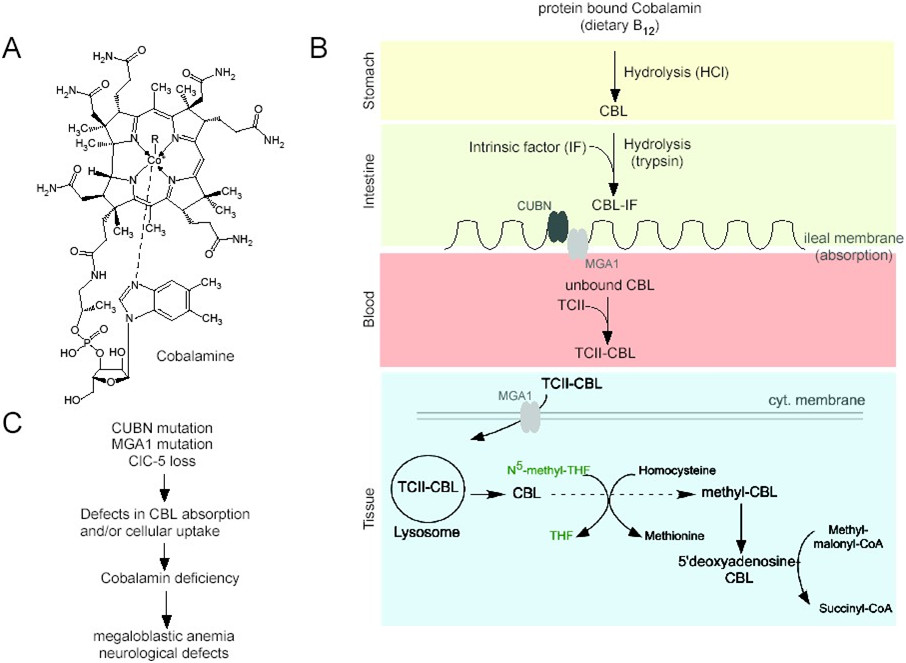
Figure 1.Structure (A) and metabolism of the vitamin B12 (B). The metabolic journey of cobalamin (cbl) from nutrient intake to its intestinal absorption. Endocytic receptors and proteins responsible for vitamin B12 intestinal absorption include cubilin (CUBN), amnionless (AMN), receptor-associated protein and megalin (MGA1). The membrane megalin/transcobalamin II (TCII)-receptor complex allows the cellular uptake of cbl. Lysosomal-mediated degradation of TCII and subsequent release of free-cbl is essential for vitamin B12 metabolic functions. MS, methonine synthase; THF, tetrahydrofolate; MTHFR, methylene tetrahydrofolate reductase; MCM, methylmalonyl CoA mutase [1,5].
References Search
A literature search was performed on the PubMed database of the US National Library of Medicine and on Scholar Google. We searched for articles published between January 2010 and June 2018, using the following key words or associations: “vitamin B12”, “cobalamin”, “vitamin B12 deficiency”, “cobalamin deficiency”, “oral vitamin B12”, “oral cobalamin”, “oral vitamin B12 therapy”, “oral cobalamin therapy”, “Biermer’s disease”, “pernicious anemia”; restrictions included: English- or French-language publications; published from January 1, 2010, to July 1, 2018; human subjects; clinical trials, review articles or guidelines.
Additional studies were obtained from references of identified studies, the Cochrane Library and the ISI Web of Knowledge. Data gleaned from international meetings were also used, as information gleaned from commercial sites on the web.
All of the English and French abstracts were reviewed by at least 2 senior researchers from our research team (CAREnce en vitamine B12 [CARE B12], in the university hospital of Strasbourg, France). After rigorous selection, only 37 papers were selected and analyzed. The latter were used to write this paper in the form of a narrative short review.
CobalaminMetabolism and its Abnormalities or Defects
Cobalamin metabolism is complex and is made up of many processes, abnormalities or defects in any one of which can lead to vitamin B12 deficiency [1]. The different stages of cobalamin metabolism and corresponding causes of cobalamin deficiency are shown in Figure 1 [4,5]. In this setting, the best known pathology is Biermer’s disease also classically know as pernicious anemia.
Biermer’s disease is an autoimmune gastritis resulting from the destruction of gastric parietal cells and consequent impairment of intrinsic factors secretion to bind the ingested vitamin B12 [4,5]. Other autoimmune disorders, especially thyroid disease, diabetes mellitus, and vitiligo, are also commonly associated with pernicious anemia.
A typical Western diet contributes 3–30 µg of vitamin B12 per day towards the recommended dietary allowance of 2.4 µg par day for adults [5]. The 5–10 year delay between the onset of vitamin B12 deficiency and the development of clinical symptoms is directly attributable to hepatic stores of cobalamin (>1.5 mg) and the enterohepatic cycle [4,5].
In the context of this paper, it is important to know that between 1–5% of “free” cobalamin or “crystalline” cobalaminis absorbed by passive diffusion along the entire gastro-intestinal tract, from the oral or nasal mucosa to the colic mucosa [4,5]. Passive diffusion accounts for about 1% of total absorption, and this route of absorption is unaffected in patients with pernicious anemia. This absorption explains the mechanism underlying oral and nasal treatment of vitamin B12 deficiencies.
In humans, cobalamin participates in 2 enzymatic processes (Figure 1) [6]. First in the methionine synthase reaction, homocysteine is converted to methionine allowing for the “recycling” of 5-methyl-tetrahydrofolate (THF) to N5,10 methylene-THF which is needed for the de novo synthesis of thymidylic acid and ultimately, for DNA formation. Concurrently, homocysteine accumulates while methionine decreases, leading to a decrease in S-adenosylmethionine which further limits N5,10-methylene-THF formation by decreasing the synthesis of formyl-THF (“formate starvation”). Decreased methionine and S-adenosylmethionine may limit many methylation reactions including those involving DNA and myelin basic protein. Second in the methylmalonyl CoA mutase reaction, methylmalonyl CoA, derived from propionic acid synthesized by intestinal bacteria, is converted to succinyl CoA, a precursor for fatty acid and heme synthesis. Thus, cobalamin deficiency results in methylmalonic acid (MMA) accumulation.
These reactions explain the main clinical manifestation of vitamin B12 deficiency: megaloblastic anemia and neuro-cognitive abnormalities [1,2]. They also explain the elements of the definition of vitamin B12 deficiency. Thus, vitamin B12 deficiency is characterized by serum vitamin B12 levels <150 pmol/L (200 pg/mL) ± serum total homocysteine levels >13 µmol/L or urinary MMA >0.4 µmol/L [7].
Manifestations and Etiologies of Vitamin B12 Deficiency in Adults
Vitamin B12 deficiency is relatively frequent in elderly patients, around 2 to more than 30% according to depending on the target population, the design and location of the studies, but is often unrecognized or not investigated because the clinical manifestations of vitamin B12 deficiency are subtle [5]. Absolute deficiency occurs up to 6% of those aged 60 years and older, whereas marginal deficiency occurs in close to 20% of patients in later life. However, certain complications of vitamin B12 deficiency, in particular psycho-neurological and hematological complications are potentially serious, as see in Table 1, and therefore require investigation in all patients who present with vitamin or nutritional deficiency.
In industrialized countries, disorders such as nutritional deficiencies, malabsorption or genetic cobalamin disorders are rare or exceptional etiologies of vitamin B12 deficiency, especially in adults [5]. In European countries, it has been estimated that the prevalence of Biermer’s disease is approximately 4% of the population. Even outside the classic Biermer’s disease, a more common problem is food-cobalaminmalabsorption (FCM), a disorder characterized by the inability to release cobalamin from food or its binding proteins [8,9]. In several recent studies, FCM and Biermer’s disease are the main causes of vitamin B12 deficiency in adults and elderlies (between 70 to 80%) [9].
In this relatively recent description syndrome of FCM, at least in its complete form, the absorption of unbound cobalamin (free or crystalline) remains within the normal range (Figure 1) [8]. The partial nature of this form of malabsorption might produce a more slowly progressive depletion of cobalamin storescompared to that seen with the more complete malabsorption engendered by disruption of intrinsic-factor-mediated absorption, as in Biermer’sdisease [8,9]. This may explain the subtle manifestations of the FCM in some patient, especially in the early stages.
The partial nature of this form of malabsorption (bound-cobalamin) explains that oral vitamin B12 may be effective to cure the deficiency. This also explains why the required treatment dose of oral vitamin B12 may be lower in FCM than in Biermer’s disease [10].
Parenteral Vitamin B12 Treatment
The classic treatment for vitamin B12 deficiency is by parenteral administration, as intramuscular (IM) injections in main countries, in the form of cyano- and, more rarely, hydroxyl- (also called hydroxo-) or methyl-cobalamin, especially for this later for the treatment of genetic deficiencies [10,11].
This mode of administration is explained by the fact that the 2 main etiologies of vitamin B12 deficiencies were historically the pernicious anemia and the malabsorption, in particular following gastrectomy for stomach ulcer [11]. Theoretically, hydroxocobalamin have several advantages due to better tissue retention and storage as demonstrated in some studies [12]. To our knowledge, it does seem not so evident in clinical practice.
However despite ancient use, the management concerning both the dose and schedule of administration varies considerably between countries [10]. This fact is related to the lack of randomized study fulfilled the criteria of evidence based-medicine in this field of medicine. In the USA and UK, doses ranging from 100 to 1,000 µg per month (or every 2-3 months when hydroxocobalamin is given) are used for the duration of the patient’s life [11]. In France, treatment involves the administration of 1,000 µg of cyanocobalamin per day for 1 week, followed by 1,000 µg per week for 1 month, followed by 1,000 µg per month, again, normally for the remainder of the patient’s lifetime [10].
Oral vitamin B12 treatment
Since cobalamin is absorbed by intrinsic factor-independent passive diffusion, daily high-dose (pharmacological dose, 1,000 to 2,000 µg per day) oral vitamin B12 (cyanocobalamin) can induce and maintain remission in patients with megaloblastic anemia [3,13]. In fact, as we have seen before, 1 to 5% of oral vitamin B12 is absorbed through passive way [4]. In this setting, alternative routes of cobalamin administration have been developed, experimented and used with good effect such as the oral [3,10,13] and nasal [14,15]. These other routes of administration have been proposed as a way of avoiding the discomfort, inconvenience and cost of monthly injections (with the need of a nurse) [16,17].
To our knowledge, at least four narrative reviews, including patients with pernicious anemia, have reported preliminary data of the efficacy of oral vitamin B12 treatment [3,10,18,19]. Although well done methodologically, results of these reviews have remained relatively confidential, without any real change in practice at the beginning of the 2000’s. This practice is however predominant in the Nordic countries. Thus, curative oral vitamin B12 treatment accounts for more than 70% of the total vitamin B12 prescribed in Sweden since the 1980s [20].
Nevertheless to date, with the dissemination of knowledge (through the Web) and thanks to the existence of good quality studies, this is changing. Thus, at least four studies that fulfilled the criteria of evidence based-medicine (randomized study, systematic review) supported the efficacy of oral vitamin B12 therapy [21-24]. In the literature, several other recent not randomized studies support the efficacy or oral vitamin B12 replacement [10,17].
Randomized Controlled Studies of Oral Vitamin B12 Therapy in Vitamin B12 Deficiency
Several prospective randomized controlled studies comparing oral vitamin B12 vs. IM vitamin B12 treatment have well-documented the efficacy (defined as the normalization and or an significant increase of the serum vitamin B12 level) and safety of oral vitamin B12 as a curative treatment [20,21,24]. Three of these currently published prospective studies include at least patients with potential Biermer’s disease (n = 18). It is to note that the treatment regime of vitamin B12 (frequency and daily dose) the oral and IM groups varied in these studies. To our knowledge, only 2 of the randomized studies have well-documented the efficacy of oral vitamin B12 therapy in term of serum vitamin B12 levels (Table 2) [21,22]. Moreover only 2 studies reported data on adverse events.
In a first study, Kuzminskiet al., in a prospective randomized trial including 38 patients (7 with pernicious anemia [18,4%]), have reported improvement of hematological parameters and vitamin B12 levels (mean value: 907 pg/mL), after 4 months of oral cyanocobalamin replacement using a much higher dose (i.e. 2,000 µg per day) (Tab. 2) [21]. In this study, serum vitamin B12 levels were significantly higher in the oral (vitamin B12 2000 μg) compared with IM (vitamin B12 1000 μg) group at 2 months: 643 ± 328 vs. 306 ± 118 pg/mL; p<0.001. The difference was even greater at 4 months: 1005 ± 595 vs. 325 ± 165 pg/mL. Four of the 18 patients in the oral group and 4 of the 15 in the IM group had a neurological response with a marked improvement or clearing of paresthesia, ataxia, or memory loss.
Bolamanet al., in a prospective randomized trial of 60 patients (11 with pernicious anemia [18,3%]), also reported significant improvement of hematological parameters and vitamin B12 levels (mean improvement: +140.9 pg/mL), after3 months of daily 1,000 µg of oral cyanocobalamin therapy (Table 2) [22]. In this study, there was an increase in serum vitamin B12 levels in both groups (oral vitamin B12 1000 μgvs. IM vitamin B12 1000 μg) at 90 days: 213.8 pg/mL in the oral and 225.5 pg/mL in the IM group. There was a statistically significant difference between days 0 and 90 in both groups (p<0.0001), but authors did not analyze difference between both groups. Both groups reported improvements of cognitive functions, sensory neuropathy, and vibration sense, but there was no statistical significant difference between both groups.
In a recent controlled, randomized, multicenter, parallel, non-inferiority clinical trial lasting one year, a preliminary analysis gives a glimpse that the oral route may be as effective and safety and more cheaply than the IM route [25]. This study involves 23 primary healthcare centers in the Madrid region (Spain), and 320 patients ≥65 years of age. In this study, IM vitamin B12 will be administered as follows: 1 mg on alternate days in weeks 1 and 2, 1 mg per week in weeks 3-8, and 1 mg per month in weeks 9-52. In the oral arm, the vitamin B12 will be administered as: 1 mg per day in weeks 1-8 and 1 mg per week in weeks 9-52. The definitive results of the Project OB12 study are expected for 2020.
In another randomized, parallel-group, double-blind, dose-finding trial, Eussenet al. showed that the lowest dose of oral cyanocobalamin required to normalize mild vitamin B12 deficiency is more than 200 timesthe recommended dietary allowance of approximately 3 µg daily (i.e. >500 µg per day) [24]. No data of the cobalamin deficiency etiology is available. Apart from helping to determine the dose, this study gives no indication for the Practitioners of the clinical effectiveness of oral vitamin B12 treatment.
It is to note that in the above studies explored the regression of the clinical manifestations (especially neurological signs) there was no relevant difference in the efficacy of oral or IM vitamin B12 administration [21,22,24]. Nevertheless to our knowledge, the effect of oral cobalamin treatment in patients presenting with severe neurological manifestations has not yet been adequately documented. Thus until this has been studied, parenteral vitamin B12 therapy is still to be recommended for such patients [26].To our knowledge, 2 of the aforementioned studies reported data on adverse events, with 2 of such adverse events in one studies in the group of oral vitamin B12 [21,22].
Systematic Reviews of Oral Vitamin B12 Therapy in Vitamin B12 Deficiency
The first evidence-based analysis by the Vitamin B12 Cochrane Group in 2005 supports the efficacy of oral vitamin B12 as a curative treatment, with a dose between 1,000 and 2,000 µg initially prescribed daily and then weekly [27]. This structured-analysis includes patients with Biermer’s disease. In this analysis, serum vitamin B12 levels increased significantly in patients receiving oral vitamin B12 and both groups of patients (receiving oral and IM treatment) showed an improvement in neurological symptoms. The Cochrane Group concludes that daily oral therapy may be as effective as IM administration in obtaining short term hematological and neurological responses in vitamin B12 deficient patients‖ [27].
The recent evidence based-analysis from the same group in 2018, also including the context of Biermer’s disease, confirms their previous analysis [23]. In fact, the Cochrane Group concludes that: “there is evidence of low quality that oral vitamin B12 or vitamin B12 administered intramuscularly have similar effects in normalizing vitamin B12 serum levels, but oral treatment costs less. Further trials should conduct better randomization and blinding procedures, recruit more participants, and provide adequate reporting. Future trials should also measure important outcomes such as the clinical signs and symptoms of vitamin B12 deficiency, health related-quality of life, socioeconomic effects, and report adverse events adequately”.
Prospective Studies of Oral Vitamin B12 Therapy in Patients with Biermer’s Disease
Our working CARE B12 group has developed an effective oral curative treatment for patients presenting with FCM and pernicious anemia using crystalline cyanocobalamin [28-32]. This treatment has been validated through several studies on small numbers of patients with a well-documented vitamin B12 deficiency, this latter of well-defined etiology. In the majority of studies, the effectiveness of treatment has been validated on the correction of serum vitamin B12 levels and that of hematological abnormalities, in general at 3 months (short term efficacy) [28-32]. In some studies, correction of neurological signs or clinical manifestations has also been sought. In all the studies, adverse events were studied.
Analysis of these data from the studies conducted by the CARE B12 group confirms the previously reported efficacy of oral crystalline cyanocobalamin, particularly inFCM and in elderly patients [28-31]. All of the patients who were treated orally corrected their vitamin B12 levels and at least two-thirds corrected their hematological abnormalities. Moreover, one-third of patients experienced a clinical improvement on oral treatment. In most cases of FCM a lowvitamin B12 dose (i.e. 125–1,000 µg of oral crystalline cyanocobalamin per day) wasused.
The aforementioned results were also observed in a population of patients presenting with Biermer’s disease (Table 3) [33]. In this setting, the CARE B12 group studied in an open study 10 patients with well-documented vitamin B12 deficiency related to pernicious anemia who daily received 1,000 µg of oral crystalline cyanocobalamin for at least 3 months [32]. After 3 months of treatment, serum vitamin B12 levels were increased in all 9 patients in whom it was measured (mean increase of 117.4 pg/mL; p<0.0000003 compared with baseline). Eight patients had increased hemoglobin levels (mean increase of 2.45 g/dL; p<0.01). All 10 patients had decreased mean erythrocyte cell volume (mean decrease of 10.4 fL; p<0.003). Three patients (one-third) experienced clinical improvements.
Two other studies have documented the efficacy of oral vitamin B12 therapy in patients with pernicious anemia (Tab. 3) [20,34]. These studies also had small sample size but had longer follow-up period (up to 18 months).
Oral vitamin B12 was effective in all the patients (10 patients had pernicious anemia) in Nyholm’s study (n=40) with the median serum vitamin B12 level of 1,193 pg/mL after 3 months of treatment (Tab. 3) [20]. It was also reported that using oral treatment did not result in any new neurological complications.
Normalization of serum vitamin B12 levels was seen in all patients (inclusive of patients with pernicious anemia) in Delpre’s study with oral (sublingual) vitamin B12 replacement (n = 18) (Tab. 3) [34]. An increase in vitamin B12 level was as much as fourfold compared with pretreatment in most patients. The mean change of 387.7 pg/mL was significant (p = 0.0001).
The CARE B12 group had also documented the long-term efficacy of oral vitamin B12 treatment, with a median follow up of 2.5 years, in a population of 22 patients including patients with pernicious anemia [35]. These preliminary findings are in accordance with the results of Roth’s study, with a median follow up of more than 4 years on oral vitamin B12 therapy [36].
The CARE B12 group also documented in a small study (10 patients) the relative efficacy of oral cyanocobalamin treatment on cognitive functions (Mini Mental State Examination score)[37].In these studies including 132 patients [28-32], only 2 of these (1.5%) reported treatment-related adverse events such as skin allergy.
Thus since the 1990’s, at least half of the patients followed in the HôpitauxUniversitaires de Strasbourg (University Hospital of Strasbourg, Strasbourg, France) with well-documented vitamin B12 deficiency were treated with oral cyanocobalamin, with a dose between 125 and 2,000 µg per day depending on whether the cause is Biermer’s disease or FCM (see Tab. 4 for the used scheme) [26]. In the Department of Internal Medicine in the aforementioned Institution (>800 patients with a documented cobalamin deficiency, median age 71 years), FCM accounts for about 60–70% of the cases of vitamin B12 deficiency in elderly patients, whereas Biermer’s disease accounted for only 15–25% [38]. All of these patients who were treated orally corrected their vitamin B12 levels and at least80% corrected their hematological abnormalities [26]. Moreover, half of the patients experienced a clinical improvement on oral treatment. It is to note that the patients presenting with severe neurological manifestations were usually excluded by our team for the oral vitamin B12 treatment. In the experience of the CARE B12 group, oral vitamin B12 treatment avoids the discomfort, inconvenience and cost of monthly injections.
Table 1. Main clinical features of cobalamin deficiency [1,2,5].
|
Hematological manifestations |
Neuro-psychiatric manifestations |
Digestive manifestations |
Other manifestations |
|---|---|---|---|
|
– Frequent: macrocytosis, neutrophil hypersegmentation, aregenerative macrocytary anemia, medullar megaloblastosis (“blue spinal cord”) – Rare: isolated thrombocytopenia and neutropenia, pancytopenia – Very rare: hemolytic anemia, thrombotic microangiopathy (presence of schistocytes) |
– Frequent: polyneuritis (especially sensitive), ataxia, Babinski’s phenomenon– Classic: combined sclerosis of the spinal cord
– Rare: cerebellar syndromes affecting the cranial nerves including optic neuritis, optic atrophy, urinary and/or fecal incontinence – Under study: changes in the higher functions, dementia, stroke and atherosclerosis (hyperhomocysteinemia), parkinsonian syndromes, depression, multiple sclerosis |
– Classic: Hunter’s glossitis, jaundice, LDH and bilirubin elevation (“intramedullary destruction”)– Debatable: abdominal pain, dyspepsia, nausea, vomiting, diarrhea, disturbances in intestinal functioning
– Rare: resistant and recurring mucocutaneous ulcers |
– Frequent:tiredness, loss of appetite
– Under study: atrophy of the vaginal mucosa and chronic vaginal and urinary infections (especially mycosis), hypofertility and repeated miscarriages, venous thromboembolic disease, angina (hyperhomocysteinemia) |
Table 2. Prospective randomized controlled studies of oral vitamin B12 treatment in patients with vitamin B12 deficiency, including patients with Biermer’s disease [21,22].
| Study characteristics (number of patients) | Therapeutic modalities | Results |
|---|---|---|
| Prospective randomized controlled studyn = 38, including 7 patient with Biermer’s disease
[21] |
Oral crystalline cyanocobalamin: 2,000 µg per day, during at least 4 months | – The mean pretreatment values for serum cobalamin, methylmalonic acid, and homocysteine were, respectively, 93 pg/mL, 3,850 nmol/L, and 37. 2 µmol/L in the oral group and 95 pg/mL, 3,630 nmol/L, and 40.0 µmol/L in the parenteral therapy group. After 4 months of therapy, the respective mean values were 1,005 pg/mL, 169 nmol/L, and 10.6 µmol/L in the oral group and 325 pg/mL, 265 nmol/L, and 12.2 µmol/L in the parenteral group (IM). The higher serum cobalamin and lower serum methylmalonic acid levels at 4 months posttreatment in the oral group vs. the parenteral group were significant, withp<0.0005 and p <0.05, respectively
– Correction of hematological and neurological abnormalities wasprompt and indistinguishable between the 2 groups |
| Prospective randomized open-label study,n = 60, , including 7 patient with Biermer’s disease
[22] |
Oral crystalline cyanocobalamin: 1,000 µg p.o. once daily for 10 days (p.o. group) or cobalamin IM: 1,000 µg once daily for 10 days (i.m. group). After 10 days, both treatments were administered once a week for 4 weeks, and after that, once a month for life | – The mean serum vitamin B12 concentration increasedsignificantly from day 0 to 90 (p<0.001).– In the p.o. group, at days 30 and 90,all hematological parameters changed significantly vs. day 0 (mean hemoglobin levels increased [bothp <0.001]; mean corpuscular volume decreased [both p <0.001]; mean white blood cell count increased [day 30, p <0.01; day 90, p <0.001]; and mean platelet count increased [both p <0.001]). Reticulocytosis was observed in all patients. These hematological parameters and the recovery patterns were similar between the 2 groups
– Neurological improvement was detected in 78% in the p.o. group and 75% inthe IM group at day 30 |
Table 3. Studies of oral vitamin B12 treatment in patients with Biermer’s disease [20,32,34,35].
| Study characteristics (number of patients) | Therapeutic modalities | Results |
|---|---|---|
| Prospective, case series of low vitamin B12 levels (n = 40), including 10 patients with Biermer’s disease[20] | Loading dose of IM vitamin B12 till vitaminB12 level reached lower 25th centile (418 pg/mL) and then converted to oral vitamin B12 1000 μg per day, during 3–18 months | – Normalization of the serum vitamin B12 levels in all patients. At 3 months, median serum vitamin B12 level of 1193 pg/mL– Noadverse-effect |
| Open prospective study of low vitamin B12 levels related to Biermer’s disease (n = 10)[32] | Oral crystalline cyanocobalamin: 1,000 µg per day, during at least 3 months | – Significant increase of serum vitamin B12 levels in 90% of the patients (mean of 117.4pg/mL– Significant increase of Hb levels (mean of 2.45 g/dL) and decrease of ECV (mean of 10.4fL)
– Improvement ofclinical abnormalities in 30% of the patients – No adverse-effect |
| Open prospective study of low vitamin B12 levels related to Biermer’s disease (n = 18)[34] | Sublingual cobalamin for 7–12 days | – Normalization of serum vitamin B12 levels. Significant mean change of 387.7 pg/mL (p = 0.0001)– Increase in vitamin B12 level as much as fourfold compared with pretreatment in most patients |
| Cohort study of low vitamin B12 levels (n = 22), including patients with Biermer’s disease [35] | Oral crystalline cyanocobalamin: 650 µg per day, during a median of 2.5 years | – Normalization of serum vitamin B12 levels in 95% of thepatients– Significant increase of Hb levels (mean of 1.1g/dL)
– Improvement of clinical abnormalities in 20% of thepatients – No adverse-effect |
Hemoglobin = Hb. Erythrocyte cell volume = ECV. MMSE = Mini Mental State Examination.
Table 4. Recommendations for oral vitamin B12 treatment [23,26].
| Biermer’s disease | Intake deficiency and food-cobalamin malabsorption | |
|---|---|---|
| Parenteral administration(intramuscular) | Cyanocobalamin:
– 1,000 µg per dayfor 1week – than 1,000 µg per week for 1month – than 1,000 µg per each month, forlife
(1,000 to 2,000 µg per day for at least 1 to 3 months in case of severe neurological manifestations) |
Cyanocobalamin:
– 1,000 µg per day for 1week – than 1,000 µg per week for 1 month – than 1,000 µg per each 1 or 3 months, until the cobalamin deficiency cause is corrected
(1,000 µg per day for at least 1 to 3 months in case of severe neurological manifestations) |
| Oral administration | Cyanocobalamin:
1,000 µg per day for life* |
Cyanocobalamin:
– 1,000 µg per day for 1 month – than 125 to 1,000 µg per day, until the cobalamindeficiency cause iscorrected* |
*: The effect of oral cobalamin treatment in patients presenting with severe neurological manifestations has not yet been adequately documented.
Perspectives and Direction of Future Research
To date in clinical practice, the majority of patients with vitamin B12 deficiency is treated with parenteral vitamin B12 administration. In fact, several studies in 2000s have documented that lifelong IM injection for replacement is still a common and usual practice. Nevertheless as early as the 1950s, there were studies suggesting that oral vitamin B12 replacement may provide adequate absorption. Nevertheless, oral vitamin B12 replacement in patients with vitamin B12 remains uncommon in clinical practice. In this setting, oral cobalamin remains the “best keep secret in medicine” [40]. In our opinion, it may be “better time to propose international recommendations” [41].
The present analysis and the experience of the CARE B12 group support the use of oral vitamin B12 replacement in clinical practice. In light of the present work, we can recommend a dose of 1,000 µg per day of oral cyanocobalamin for life in case of Biermer’s disease (Tab. 4) [23,26]. In case of intake deficiency or food-cobalaminmalabsorption, we can recommend 1,000 µg per day of oral cyanocobalamin for 1 month and than 125 to 1,000 µg per day, until the cobalamin deficiency cause is corrected. In this setting, the following can also be proposed: ongoing supplementation is needed until any associated disorders are corrected (e.g. by halting the ingestion of the offending medication or exogenesis, or by treating Helicobacter pylori infection or pancreatic exocrine failure) [9,26]. This may result in lifelong administration or, when applicable, sequential administration.
The effect of oral vitamin B12 treatment in patients presenting with severe neurological manifestations has not yet been adequately documented [23,26]. Patients with vitamin B12 deficiency who are symptomatic have severe neurological deficits or have critically low blood levels of vitamin B12 should be treated with IM replacement. This is to ensure rapid replenishment of body stores to prevent irreversible consequences of the cobalamin deficiency. Subsequently, patients may be able to convert to oral replacement with close monitoring.
In clinical practice, one of the predominant elements for the choice of treatment options is the patient preference [26,42]. This latter should absolutely be taken into consideration. Other factors of this choice (IM vs. oral) include patient compliance and patient comorbidities. Thus in patients with non-compliance to oral medication, IM route may be a better option to ensure timely administration. On the other hand, oral replacement may improve adherence for patients who prefer oral medication to injections. In patients, whereby IM injections are contraindicated because of coagulopathy or the use anti-coagulation and/or anti-platelet medication, oral replacement is the best option. In this setting, oral replacement will also be useful in patients who are averse to injection. For elderly patients with sarcopenia, injections can painful and difficult to administer. In this setting, surveys on patients’ preferences for oral or IM replacement would be informative to guide clinical decision-making.
Funding
Our research on vitamin B12 deficiency was supported by a grant from the Fondation de France (Prix Robert et Jacqueline Zittoun 2004).
Competing Interests
The authors have no conflicts of interest that are directly relevant to the content of this manuscript.
Authors Contribution
Conceived and designed the study: EA and AAZ. Performed the study: EA, AAZ and TV.Analyzed the data: EA and AAZ.Interpreted the results: EA and AAZ.Wrote the paper: EA and AAZ. Principal Investigator of this study and supervised this study: EA. Revised the paper critically and give final approval for publication: all authors.
References
Herrmann W, Obeid R. Cobalamin deficiency. 2012;56:301-22.
Dali-Youcef N, Andrès E. An update on cobalamin deficiency in QJM. 2009;102:17-28.
Lane LA, Rojas-Fernandez C. Treatment of vitamin B12 deficiency anemia: oral versus parenteral therapy. Ann Pharmacother. 2002;36:1268-72.
Hvas AM, Nexo E. Diagnosis and treatment of vitamin B12 deficiency: an update. Haematologica. 2006;91:1506-12.
Andrès E, Loukili NH, Noel E, et al. Vitamin B12 (cobalamin) deficiency in elderly patients. CAMJ. 2004;171:251-60.
Green R, Allen LH, Bjørke-Monsen AL, et al. Vitamin B12 deficiency. Nat Rev Dis Primers. 2017;3:17040.
Chatthanawaree W. Biomarkers of cobalamin (vitamin B12) deficiency and its application. J Nutr Health Aging. 2011;15:227-31.
Carmel R. Malabsorption of food- cobalamin. Bailliere’sClinHaematol. 1995;8:639-55.
Andrès E, Affenberger S, Vinzio S, et al. Food-cobalaminmalabsorption in elderly patients: clinical manifestations and treatment. Am J Med. 2005;118:1154-59.
Andrès E, Dali-Youcef N, Vogel T, et al. Oral cobalamin (vitamin B12) treatment. An update. IntJnl Lab Hem. 2009;31:1-8.
Lee GR. Pernicious anemia and other causes of vitamin B12 (cobalamin) deficiency. In: Lee GR, et al., eds. Wintrobe’s Clinical Hematology. 10th ed. Baltimore: Williams & Wilkins, 1999:941-64.
Arendt J, Nexø E. Treatment response in vitamin B12 deficiency depends on the chosen vitamin B12 preparation. UgeskrLaeger. 2011;173:2634-5.
Elia M. Oral or parenteral therapy for B12 deficiency. Lancet. 1998;352:1721-22.
Slot WB, Merkus FW, Van Deventer SJ, et al. Normalization of plasma vitamin B12 concentration by intranasal hydroxocobalamin in vitamin B12-deficient patients. Gastroenterology. 1997;113:430-33.
van Asselt DZ, Merkus FW, Russel FG, Hoefnagels WH. Nasal absorption of hydroxocobalamin in healthy elderly adults. Br J ClinPharmacol. 1998;45:83-6.
Masucci L, Goeree R. Vitamin B12 intramuscular injections versus oral supplements: a budget impact analysis. Ont Health Technol Assess Ser. 2013;13:1-24.
Castelli MC, Friedman K, Sherry J, et al. Comparing the efficacy and tolerability of a new daily oral vitamin B12 formulation and intermittent intramuscular vitamin B12 in normalizing low cobalamin levels: a randomized, open-label, parallel-group study. ClinTher. 2011;33:358-371.e2.
Lin J, Kelsberg G, Safranek S. Clinical inquiry: Is high-dose oral B12 a safe and effective alternative to a B12 injection? J FamPract. 2012;61:162-3.
Butler CC, Vidal-Alaball J, Cannings-John R, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: a systematic review of randomized controlled trials. FamPract. 2006;23:279-85.
Nyholm E, Turpin P, Swain D, et al. Oral vitamin B12 can change our practice. Postgrad Med J. 2003;79:218-9.
Kuzminski AM, Del Giacco EI, Allen RH, et al. Effective treatment of cobalamin deficiency with oral cobalamin. Blood. 1998;92:1191-98.
Bolaman Z, Kadikoylu G, Yukselen V, et al. Oral versus intramuscular cobalamin treatment in megaloblastic anemia: a single-center, prospective, randomized, open-label study. ClinTher. 2003;25:3124-34.
Wang H, Li L, Qin LL, Song Y, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst Rev. 2018 Mar 15;3:CD004655.
Eussen SJ, de Groot LC, Clarke R, et al. Oral cyanocobalamin supplementation in older people with vitamin B12 deficiency: a dose-finding trial. Arch Intern Med. 2005;165:1167-72.
Sanz-Cuesta T, González-Escobar P, Riesgo-Fuertes R, et al. Oral versus intramuscular administration of vitamin B12 for the treatment of patients with vitamin B12 deficiency: a pragmatic, randomised, multicentre, non-inferiority clinical trial undertaken in the primary healthcare setting (Project OB12). BMC Public Health. 2012;12:394.
Andrès E, Fothergill H, Mecili M. Efficacy of oral cobalamin (vitamin B12) therapy. Expert Opinion Pharmacotherapy. 2010;11:249-56.
Vidal-Alaball J, Butler CC, Cannings-John R, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst Rev. 2005; 20: CD004655.
Andrès E, Kurtz JE, Perrin AE, et al. Oral cobalamin therapy for the treatment of patients with food-cobalaminmalabsorption. Am J Med. 2001;111:126-29.
Andrès E, Kaltenbach G, Noel E, et al. Efficacy of short-term oral cobalamin therapy for the treatment of cobalamin deficiencies related to food-cobalaminmalabsorption. A study of 30 patients. Clin Lab Haematol. 2003;25:161-66.
Kaltenbach G, Noblet-Dick M, Andrès E, Barnier-Figue G, et al. Réponse précoce au traitement oral par vitamine B12 chez des sujets âgés hypovitaminiques. Ann Med Interne (Paris). 2003;154:91-5.
Andrès E, Kaltenbach G, Noblet-Dick M, et al. Hematological response to short-term oral cyanocobalamin therapy for the treatment of cobalamin deficiencies in elderly patients. J Nutr Health Aging. 2006;10:3-6.
Andrès E, Loukili NH, Noel E, et al. Oral cobalamin (daily dose of 1000 µg) therapy for the treatment of patients with pernicious anemia. An open label study of 10 patients. CurrTher Research. 2005;66:13-22.
Andrès E. Oral Cobalamin Therapy for the Patient with Biermer’s Disease. J Blood DisordTransfus. 2017;8:1.
Delpre G, Stark P, Niv Y. Sublingual therapy for cobalamin deficiency as an alternative to oral and parenteral cobalamin supplementation. Lancet. 1999;354:740–1.
Andrès E, Serraj K, Federici L, et al. Efficacité au long cours d’un traitement par cyanocobalamine administrée par voie orale dans le cadre des carences en vitamine B12: étude de 22 cas. Rev Med Interne. 2007;28(suppl. 1):49.
Roth M, Orija I. Oral vitamin B12 therapy in vitamin B12 deficiency. Am J Med. 2004;116:358.
Jehl C, Vogel T, Andrès E, Kaltenbach G. Benefits of oral cobalamin on cognitive function in elderly persons with vitamin B12 deficiency. Geriatrics World Congress, Paris, June 2009.
Andrès E, Goichot B, Schlienger JL. Food-cobalaminmalabsorption: a usual cause of vitamin B12 deficiency. Arch Intern Med. 2000;160:2061-62.
Vitetta L, Zhou J, Manuel R, et al. Route and type of formulation administered influences the absorption and disposition of vitamin B12 levels in serum. J. Funct. Biomater. 2018;12: 1-9.
Graham ID, Jette N, Tetroe J, et al. Oral cobalamin remains medicine’s best kept secret. Arch GerontolGeriatr. 2007;44:49-59.
Andrès E. Oral cobalamin therapy: it may be perhaps time to propose international recommendations ? Presse Med. 2012;41:895-8.
Chan CQ, Low LL, Lee KH. Oral vitamin B12 replacement for the treatment of pernicious anemia. Frontiers in Medicine. 2016;3:1-6.
Received: July 18, 2018;
Accepted: August 17, 2018;
Published: August 21, 2018.
To cite this article : Andrès E, Abrar Z, Vogel T. State of Art of Oral Vitamin B12 (Cobalamin) in Biermer’s Disease (Pernicious Anemia). Japan Journal of Medicine. 2018: 1:6.
©Andrès E, et al. 2018.
